Cutaneous T-cell lymphomas (CTCL)
CTCLs are rare, heterogeneous types of non-Hodgkin T-cell lymphoma that primarily manifest in the skin but can involve other disease compartments.1
CTCLs include a spectrum of variants. Mycosis Fungoides and Sézary Syndrome together are the most common CTCL subtypes.1,2
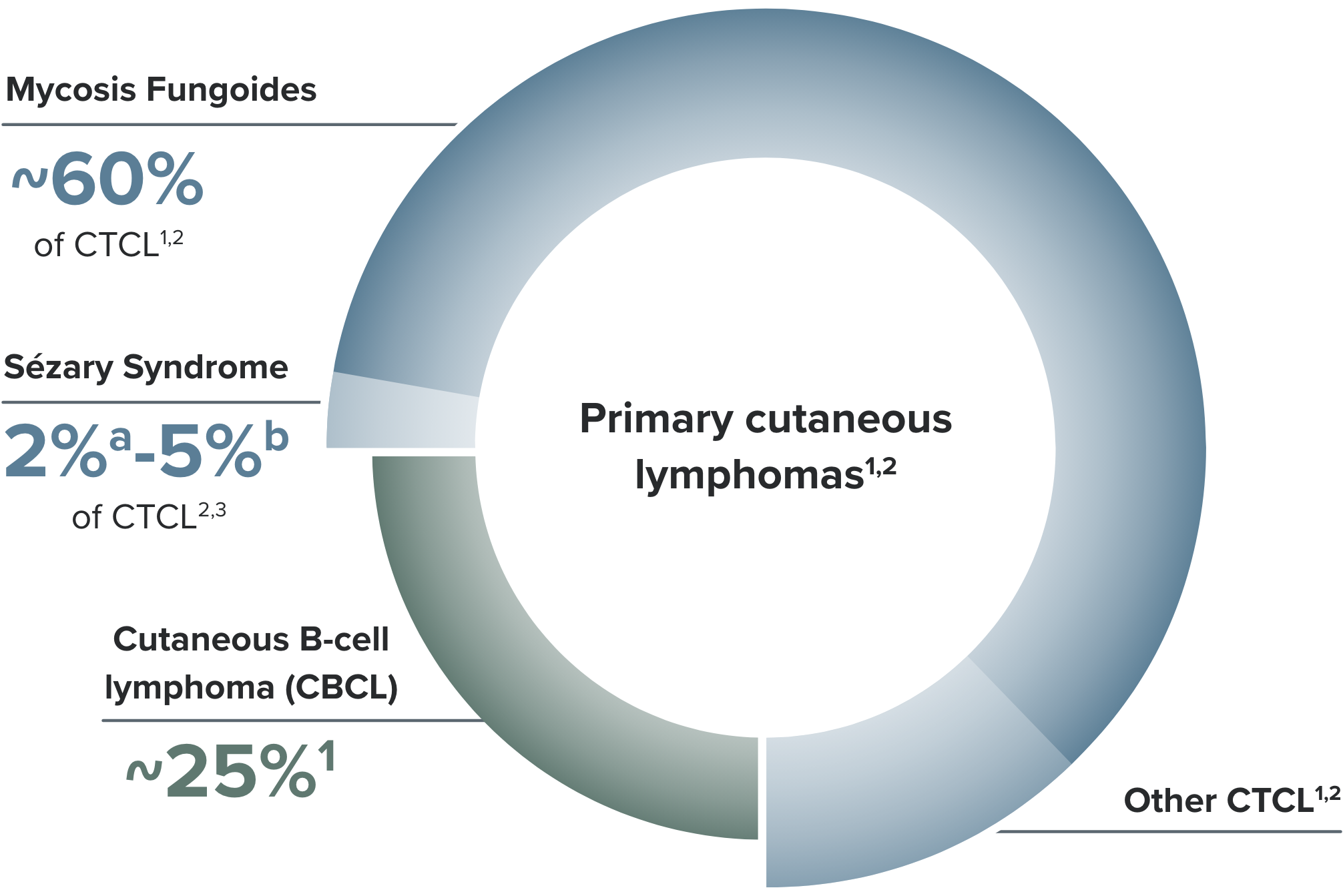
- aIncidence rate in 18 SEER registries between 2000-2018.3
- bBased on SEER database neoplasm information that summarizes results of reportable cases diagnosed in 1978 and later.3
Consulting with CTCL experts is recommended
For optimal management of Mycosis Fungoides and Sézary Syndrome, NCCN Guidelines recommend4:
- Working with a multidisciplinary team of specialists with expertise in CTCL, including a hematologist-oncologist, dermatologist, pathologist, and radiation oncologist
- Consultation and/or treatment at centers with expertise in managing CTCL
- Referral to a pathologist with expertise in CTCL for evaluation of skin and nodal biopsies

Mycosis Fungoides
Mycosis Fungoides presentation includes persistent skin lesions of varying sizes and shapes.5 It is often indolent or slowly progressive, and in many cases is limited to the skin.5,6
However, up to 1 in 3 patients with Mycosis Fungoides may experience progression within skin or to other compartments,7,a and progression from early to more advanced-stage Mycosis Fungoides is associated with decreased survival.8
- aBased on a survival outcomes and prognostic factors study that included 1502 patients with Mycosis Fungoides/Sézary Syndrome.3
Clinical characteristics
Clinical characteristics of Mycosis Fungoides are heterogeneous5 and include:
- Patches, plaques, tumors, and erythroderma
- May mimic other inflammatory skin diseases5
Examples of Mycosis Fungoides symptoms
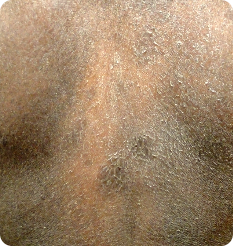
Patchesa
- Most common initial skin lesions—flat, scaly patches of varying sizes, shapes, and colors5
- Most prevalent on sun-protected sites (eg, hips and buttocks)9
- Images are intended to be an example. Actual presentation can vary depending on individual patient factors.
- aPhotos courtesy of Oleg Akilov, MD, PhD.
Plaquesa
- Plaques may develop with localized or generalized distribution—small raised bumps or thick hard lesions that may have a scaly texture5
- Well-defined, firm, raised lesions; smooth or scaly texture10
- Images are intended to be an example. Actual presentation can vary depending on individual patient factors.
- aPhotos courtesy of Oleg Akilov, MD, PhD.
Tumorsa
- Patients with history of plaque disease may develop ulcerated or exophytic tumors5
- Dome-shaped raised growths, which may be ulcerated and painful6
- Images are intended to be an example. Actual presentation can vary depending on individual patient factors.
- aPhotos courtesy of Oleg Akilov, MD, PhD.
Combination Lesions
- Lesion types may present in combination7
- Images are intended to be an example. Actual presentation can vary depending on individual patient factors.
- aPhoto courtesy of Oleg Akilov, MD, PhD.
- bImage used with permission from Semin Cutan Med Surg.
Unusual Variants
- Unusual variants may be seen6,11
- Images are intended to be an example. Actual presentation can vary depending on individual patient factors.
- aPhoto courtesy of Oleg Akilov, MD, PhD.
- bImage used with permission from Dermatol Pract Con.
- cImages used with permission from Lauren Hughey, MD.
- Most common initial skin lesions—flat, scaly patches of varying sizes, shapes, and colors5
- Most prevalent on sun-protected sites (eg, hips and buttocks)9
- Images are intended to be an example. Actual presentation can vary depending on individual patient factors.
- aPhotos courtesy of Oleg Akilov, MD, PhD.
- Plaques may develop with localized or generalized distribution—small raised bumps or thick hard lesions that may have a scaly texture5
- Well-defined, firm, raised lesions; smooth or scaly texture10
- Images are intended to be an example. Actual presentation can vary depending on individual patient factors.
- aPhotos courtesy of Oleg Akilov, MD, PhD.
- Unusual variants may be seen6,11
- Images are intended to be an example. Actual presentation can vary depending on individual patient factors.
- aPhoto courtesy of Oleg Akilov, MD, PhD.
- bImage used with permission from Dermatol Pract Con.
- cImages used with permission from Lauren Hughey, MD.

Sézary Syndrome
Sézary Syndrome is a leukemic subtype of CTCL. It is characterized by the presence of atypical T cells (Sézary cells) in skin and erythema over 80% or more of the skin, with a high level of blood involvement (B2 classification).9
Other symptoms may include9,13:
- Lymphadenopathy
- Pruritus
- Skin erosions
- Alopecia
- Nail abnormalities
- Hyperkeratosis
- Ocular abnormalities (eg, ectropion)
Patients with Sézary Syndrome are also prone to skin infection, partly due to immunosuppression, with a high mortality risk due to opportunistic infection.5,14
Examples of Sézary Syndrome symptoms
- aImages adapted from photos provided courtesy of Dr. Oleg Akilov, University of Pittsburgh.
- bImage adapted from photos provided courtesy of Dr. Joan Guitart, Northwestern University.
Explore videos for Mycosis Fungoides and Sézary Syndrome
Understanding CTCL
Challenges in diagnosis
Early-stage Mycosis Fungoides
References: 1. Willemeze R, Cerroni L, Kemf W, et al. The 2018 update of the WHO-EORTC classification for primary cutaneous lymphomas. Blood. 2019;133:1703-1714. 2. Cai ZR, Chen ML, Weinstock MA, Kim YH. Incidence trends of primary cutaneous T Cell lymphoma in the US from 2000 to 2018: a SEER population data analysis. JAMA Oncol. 2022;8(11):1690-1692. 3. National Institutes of Health - National Cancer Institute. SEER Program - Sezary syndrome. https://seer.cancer.gov/seertools/hemelymph/51f6cf56e3e27c3994bd52e2/?q=sezary%20syndrome. Accessed September 18, 2023. 4. Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Primary Cutaneous Lymphomas V2.2025. © National Comprehensive Cancer Network, Inc. 2024. All rights reserved. Accessed September 6, 2024. To view the most recent and complete version of the guideline, go online to NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way. 5. Hoppe RT, Kim YH. Clinical manifestations, pathologic features, and diagnosis of mycosis fungoides. UpToDate. https://www.uptodate.com/contents/clinical-manifestations-pathologic-features-and-diagnosis-of-mycosis-fungoides. Updated September 19, 2024. Accessed December 18, 2024. 6. Scarisbrick JJ, Quaglino P, Prince HM, et al. The PROCLIPI international registry of early-stage mycosis fungoides identifies substantial diagnostic delay in most patients. Br J Dermatol. 2019;181(2):231-232. 7. Agar NS, Wedgeworth E, Crichton S, et al. Survival outcomes and prognostic factors in mycosis fungoides/Sézary syndrome: validation of the revised International Society for Cutaneous Lymphomas/European Organisation for Research and Treatment of Cancer staging proposal. J Clin Oncol. 2010;28(31):4730-4739. 8. Allen PB, McCook AA, Switchenko JM, et al. Staging lymph nodes and blood at diagnosis in mycosis fungoides identifies patients at increased risk of progression to advanced stage: A retrospective cohort study. Cancer. 2023;129:541-550. 9. Willemeze R, Jaffe ES, Burg G, et al. WHO-EORTC classification for cutaneous lymphomas. Blood. 2005;105:3768-3785. 10. National Cancer Institute. Mycosis fungoides plaque. Accessed March 10, 2025. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/mycosis-fungoides-plaque 11. Virmani P, Myskowski PL, Pulitzer M. Unusual variants of mycosis fungoides. Dian Histopath (Oxf). 2016;21(22):142-151. 12. Olsen EA, Whittaker S, Willemeze R, et al. Primary cutaneous lymphoma: recommendations for clinical trial design and staging update from the ISCL, USCLC, and EORTC. Blood. 2022;140(5):419-437. 13. Jawed SI, Myskowski PL, Horwitz S, et al. Primary cutaneous T-cell lymphoma (mycosis fungoides and Sézary syndrome) Part I. Diagnosis: Clinical and histopathologic features and new molecular and biologic markers. J Am Acad Dermatol. 2014;70(2):e1-e16. 14. Rook AH, Olsen EA. Clinical presentation, pathologic features, and diagnosis of Sézary syndrome. UpToDate. https://www.uptodate.com/contents/clinical-presentation-pathologic-features-and-diagnosis-of-sezary-syndrome. Updated July 28, 2023. Accessed December 18, 2024. 15. Ogilvie C, Jackson R, Leach M, McKay P. Sezary syndrome: diagnosis and management. J R Coll Physicians Edinb. 2012;42(4):317-321. 16. Spicknall KE. Sézary syndrome-clinical and histopathologic features, differential diagnosis, and treatment. Semin Cutan Med Surg. 2018;37(1):18-23.